HEDIS Information

Molina Healthcare of Florida uses the Healthcare Effectiveness Data and Information Set (HEDIS®) tool each year as a way to measure quality. This is done by looking at the type of care and services provided. HEDIS® is maintained by the National Committee for Quality Assurance (NCQA). This allows the review of certain aspects of care. This includes clinical and non-clinical care. It also shows where plans can improve care and service. Molina’s goal is to be better than 75% of other Medicaid health plans in the nation.
Medicaid HEDIS® Annual Rates.
Molina’s scores for the past two years are below. You can see how Molina performs compared to the NCQA 66.67th percentile Quality Compass Benchmark.
The HEDIS reporting year is the year after the data was collected. For example, “2024 Rate” includes data from January to December 2023 and “2025 Rate” includes data from January to December 2024.
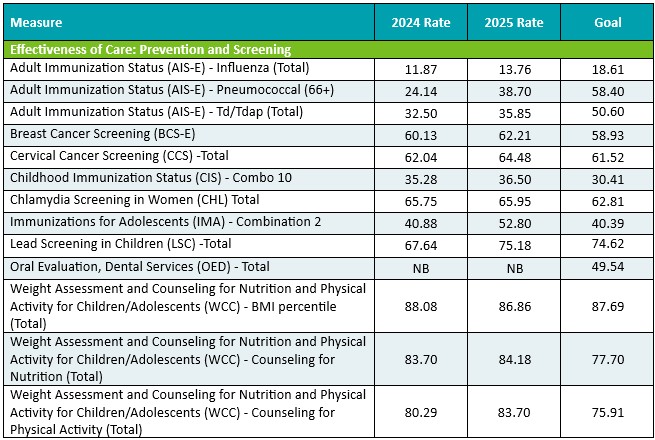


NB = No Benefit
If you have questions or would like additional information about HEDIS®, please contact Molina Healthcare of FL Quality Department at (866) 472-4585 (TTY: 711). You may request printed copies of all content posted on our website by calling the Member Services number on your member ID card.
HEDIS® is a Registered Trademark of the National Committee for Quality Assurance.


