2023 Medicaid Renewals
 The Medicaid redetermination (aka, renewal) processes has resumed for the first time since February 2020—just before the COVID Public Health Emergency. Now, Medicaid members must renew their benefits in order to retain health coverage and continue to receive uninterrupted care.
The Medicaid redetermination (aka, renewal) processes has resumed for the first time since February 2020—just before the COVID Public Health Emergency. Now, Medicaid members must renew their benefits in order to retain health coverage and continue to receive uninterrupted care.
Providers are encouraged to use this information to help educate your Medicaid and MMP/Duals patients on the importance of updating their contact information and how this affects renewal of their Medicaid coverage.
Frequently Asked Questions (FAQs)
When Medicaid redeterminations resume, most Medicaid recipients will need to go through a redetermination, or renewal, process to keep their Medicaid eligibility and benefits. We need your help to ensure your Medicaid patients don’t lose coverage.
Q: When will the normal Medicaid enrollment and renewal process resume?
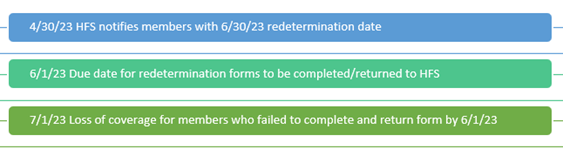
A: The Centers for Medicare & Medicaid Services (CMS) has provided guidance requiring all state Medicaid agencies to resume redetermination activities by April 30, 2023, for members with a redetermination date of June 30, 2023. This cycle will repeat each month.
Q: What can individuals (Medicaid recipients) do to prepare?
A: First and foremost, all Medicaid recipients should make sure their contact information, including their mailing address and phone number(s), are up to date with HFS to ensure they receive important notices about the renewal process.
- Learn how our members can update their contact information with the HFS and Molina online at illinois.gov/hfs/MedicalClients/Pages/addresschange.aspx.
- Ask our members—your patients—to make sure they keep an eye out for information and notices about their coverage and renewal process, and respond promptly to any instructions they receive.
- Learn more about the renewal process for members and the assistance available to them online at MolinaHealthcare.com/KeepMyHealthPlan/IL.
Q: What happens if an individual is no longer eligible for Medicaid and loses coverage?
A: If an individual no longer qualifies for Medicaid coverage through HFS, they will receive:
- A notice in the mail with the date their Medicaid coverage will end.
- Information on how to file an appeal, if they think the decision to cancel their coverage was incorrect.
Q: What are some other choices for health coverage if an individual no longer qualifies for Medicaid?
A: Individuals should contact HFS to see what other options are available. If a member no longer qualifies for Medicaid, they may be eligible for a Marketplace or Medicare health plan.
- To learn more about our Marketplace plans, visit MolinaMarketplace.com or call (844) 802-7472.
- To learn more about our Medicare health plan, visit MolinaMedicare.com or call (866) 403-8293.
Q: How do I determine if my patient is currently covered by Medicaid?
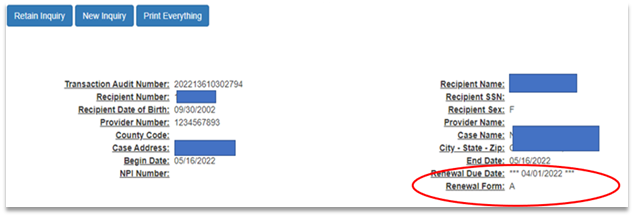
A: Providers can use the HFS tool known as the Medical Electronic Data Interchange (MEDI) System, which shows both the redetermination date and the form type the member will be receiving.
Providers can also log onto the Availity Essentials portal to search for a member's redetermination status. This Quick Reference Guide will show you how.
Q: What are the form types?
A: Each member will receive one of two different form types for redeterminations:
- Form A: Income has been automatically validated and member is not required to return form. Coverage will automatically continue. This process is called “ex parte.”
- Form B: Member is required to complete the form and respond to the redetermination for income and household verification. Failure to do so will cause the member to lose coverage. Example as seen in MEDI:
Q: How can members respond with the completed form?
A: They have three options:
- Online: Manage My Case at Illinois.gov (preferred and fastest method)
- Phone: Call the State of Illinois at (877) 805-5312
- Mail:
- This process will take the longest.
- Forms will be barcoded specific to the member and will be scanned in once received.
Q: Does HFS have a timeline for this process?
A: Yes: This cycle will continue monthly going forward.
Q: Will Molina Healthcare of Illinois be offering providers any additional redetermination guidance?
A: Yes, our team has developed a webinar with a Q&A/Discussion session. The webinar will be held several times this year. We will send an email with the registration links as soon as it’s available. Note: Only providers and staff who register to receive our Molina provider updates, which are curated specifically for providers in Illinois, will receive the email. Register for provider updates.
Q: How can I get more information about the restart of the redetermination process?
A: Contact Molina’s Provider Network Management team at (855) 866-5462 if you have any questions or would like more information.
Medicaid members can visit MolinaHealthcare.com/KeepMyHealthPlan/IL or call Molina Healthcare of Illinois at (855) 687-7861 (TTY: 711).
Q: What if I still have questions?
A: Visit the HFS website at Medical Providers (illinois.gov).
*appropriations.senate.gov/imo/media/doc/JRQ121922.PDF
