Next Generation of Ohio Medicaid's Managed Care Program
Ohio Medicaid's managed care plans
Ohio Medicaid’s managed care plans are designed to provide personalized care to meet your healthcare needs. You can explore the managed care plans available and enroll by visiting www.ohiomh.com or by contacting the Ohio Medicaid Consumer Hotline at 800-324-8680 (TTY 711). Representatives are available 7 a.m.-8 p.m. Monday through Friday and 8 a.m.-5 p.m. Saturday, Eastern Time. They can provide interpreters and answer member questions about open enrollment.
Attention Molina Healthcare members: exciting changes to Ohio’s Medicaid program effective February 1, 2023
The Next Generation managed care plans have been implemented to provide personalized benefits to members which best fit their individual healthcare needs. The Next Generation program is designed to address health inequities and disparities and achieve optimal outcomes for the holistic well-being of individuals receiving Medicaid.
The Next Generation managed care plan changes do not apply to the MyCare Ohio program, which will continue to provide benefits to Ohioans who receive both Medicaid and Medicare benefits, with enhanced coordination of medical, behavioral, and long-term care services.
Ohio Medicaid managed care members should have received a Next Generation Ohio Medicaid managed care member ID card prior to February 1, 2023, from Molina Healthcare. On February 1, 2023, members should have begun using that card when going to the pharmacy or their physician.
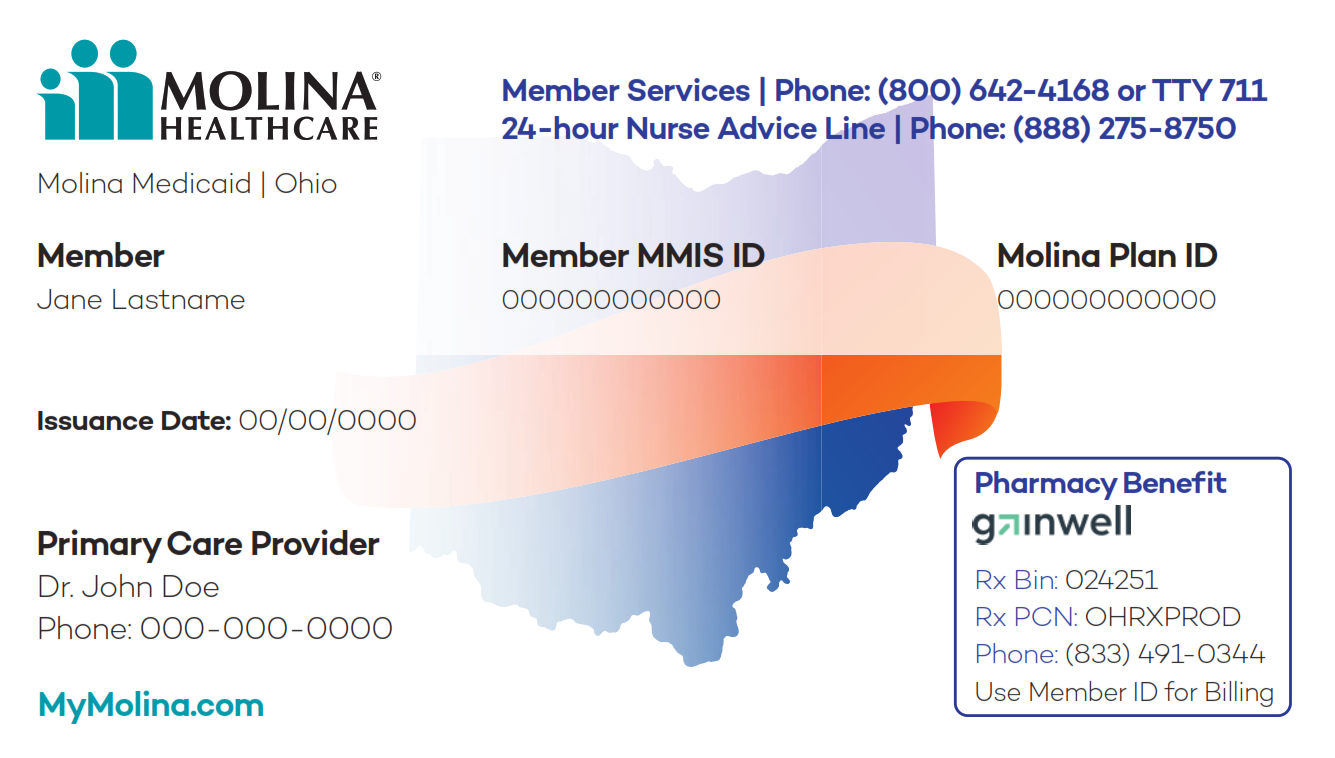
If a member hasn't received a new member ID card, they can still receive services and have prescriptions filled. Members should bring their old ID card with them to the provider or pharmacy and contact Molina Healthcare Member Services at (800) 642-4168 from Monday to Friday, 7 a.m. to 8 p.m. ET to learn more about how to print their card or access an electronic version. Members can also view and print their member ID card by logging in to their My Molina member portal online or on the My Molina mobile app.
If a member needs to request a new member ID card, please contact Molina Healthcare at (800) 642-4168 from Monday to Friday, 7 a.m. to 8 p.m. ET to learn more about how to print your card or access an electronic version. Members can also view and print their member ID card by logging in to their My Molina member portal online or on the My Molina mobile app.
Ohio Medicaid managed care members are encouraged to visit https://managedcare.medicaid.ohio.gov/individuals for additional resources and information about the latest launch of Ohio Medicaid’s Next Generation program.
Help desks are available:
- If a member has a question about Medicaid managed care eligibility, coverage, benefits, managed care plan selection, or something else, contact the Ohio Medicaid Consumer Hotline at (800) 324-8680.
- If a member has questions about their Next Generation managed care plan member ID card, contact Molina Healthcare Member Services at (800) 642-4168 from Monday to Friday, 7 a.m. to 8 p.m. ET.
Member resources:


